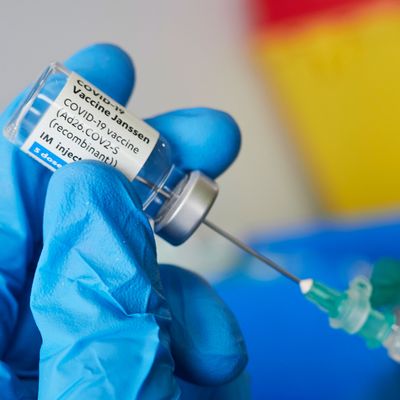
This week, the FDA announced that it would attach a warning to the Johnson & Johnson COVID-19 vaccine pertaining to its very slightly elevated risk association with Guillain-Barré syndrome, a rare neurological disorder. The announcement came after approximately 100 suspected cases were identified among the more than 12 million people who’ve received the Johnson & Johnson vaccine thus far. In April, distribution of the J&J vaccine was briefly “paused” due to concerns about a rare blood-clotting disorder; the shot was reinstated after a safety review concluded the side effect was extremely rare. As the FDA reaffirmed that “the known and potential benefits clearly outweigh the known and potential risks,” there is no reason to believe the Johnson & Johnson vaccine will be paused again.
The Cut spoke to David Putrino, a neuroscientist and director of rehab innovation at Mount Sinai, to learn more about Guillain-Barré as it pertains to the Johnson & Johnson vaccine.
What is my risk of contracting Guillain-Barré syndrome?
Given the numbers we have so far, says Putrino, one’s risk of developing Guillain-Barre syndrome (or GBS) as a result of the Johnson & Johnson vaccine amounts to 100 in 12.8 million, or roughly 0.0008 percent. “This is incredibly rare,” says Putrino. “Your likelihood of serious illness or death from COVID is still much higher than your chance of contracting GBS from the COVID vaccine, and your chance of [getting] long COVID is certainly much higher than your chance of contracting GBS from a vaccine.”
What is Guillain-Barré syndrome?
While it is incredibly unlikely that any one recipient of the Johnson & Johnson vaccine will develop GBS, Putrino classifies GBS as a serious side effect, given the length of time it takes to recover. The disorder is typically experienced as pins and needles in the extremities (usually in the feet, says Putrino, though it can begin in the hands and face), followed by progressive weakening of the muscles.
“For many people, it’s experienced as a progressive loss of voluntary movement,” Putrino explains. “Their muscles stop reacting to commands, and they feel that they can’t move.” In severe cases, patients may be temporarily bedridden, and in very, very rare cases, patients may need the assistance of mechanical ventilation due to extreme weakness.
GBS is typically treated with a combination of time and physical therapy. The duration of the disorder is often a function of the severity of the initial symptoms; milder cases may resolve in a month, while more severe cases may take six to eight months. “Once the immune response that is attacking your peripheral nerves slows to a halt, the nerves begin to regenerate, so you slowly get all of your lost function back,” says Putrino. “In the vast majority of cases, with physical therapy and rehabilitation, patients return to where they were pre-illness.”
But again, Putrino emphasizes, “This is a small part of what your body goes through when it actually gets COVID. The risks do not outweigh the benefits of the vaccine.”
Why might the J&J vaccine cause Guillain-Barré?
As mentioned above, GBS can occur as the result of an extreme immune response, and in fact is a known potential side effect associated with other vaccines, including the flu shot, says Putrino. For that reason, it’s unsurprising that it’s been found to be a very rare side effect here, too. Several thousand people in the United States develop the disorder each year (from vaccines or otherwise), and most recover completely. There is no known increased risk of GBS associated with either the Pfizer or Moderna vaccines, which rely on a different technology.
While it’s been reported that most of the reported cases of GBS tied to the Johnson & Johnson vaccine were in men aged 50 or older, we don’t have enough data to predict who may be more or less likely to develop GBS as a result of the J&J vaccine, says Putrino. “There have been less than a 100 cases so far and 12-plus million doses, so that makes it very hard to have any statistically significant understanding,” he says. “What we can say from other vaccine-mediated GBS is that we’ve never really observed a particular trend. It appears to be more random.”
What should I do if I think I have GBS?
If you’ve received the Johnson & Johnson vaccine within the last month and are now experiencing worsening weakness in your extremities, it’s certainly worth seeing a doctor immediately says Putrino — mainly, he says, “because there are far more probable causes that are far more scary, such as stroke.” Typically, GBS is diagnosed clinically, meaning the doctor will be able to observe it in the patient. In some cases, a spinal tap may be required to confirm the diagnosis. “Around 90 percent of people with GBS will have elevated levels of protein in their cerebrospinal fluid, which can be measured by doing a spinal tap,” Putrino explains.


